Understanding ADHD vs ADD: What’s the Difference?
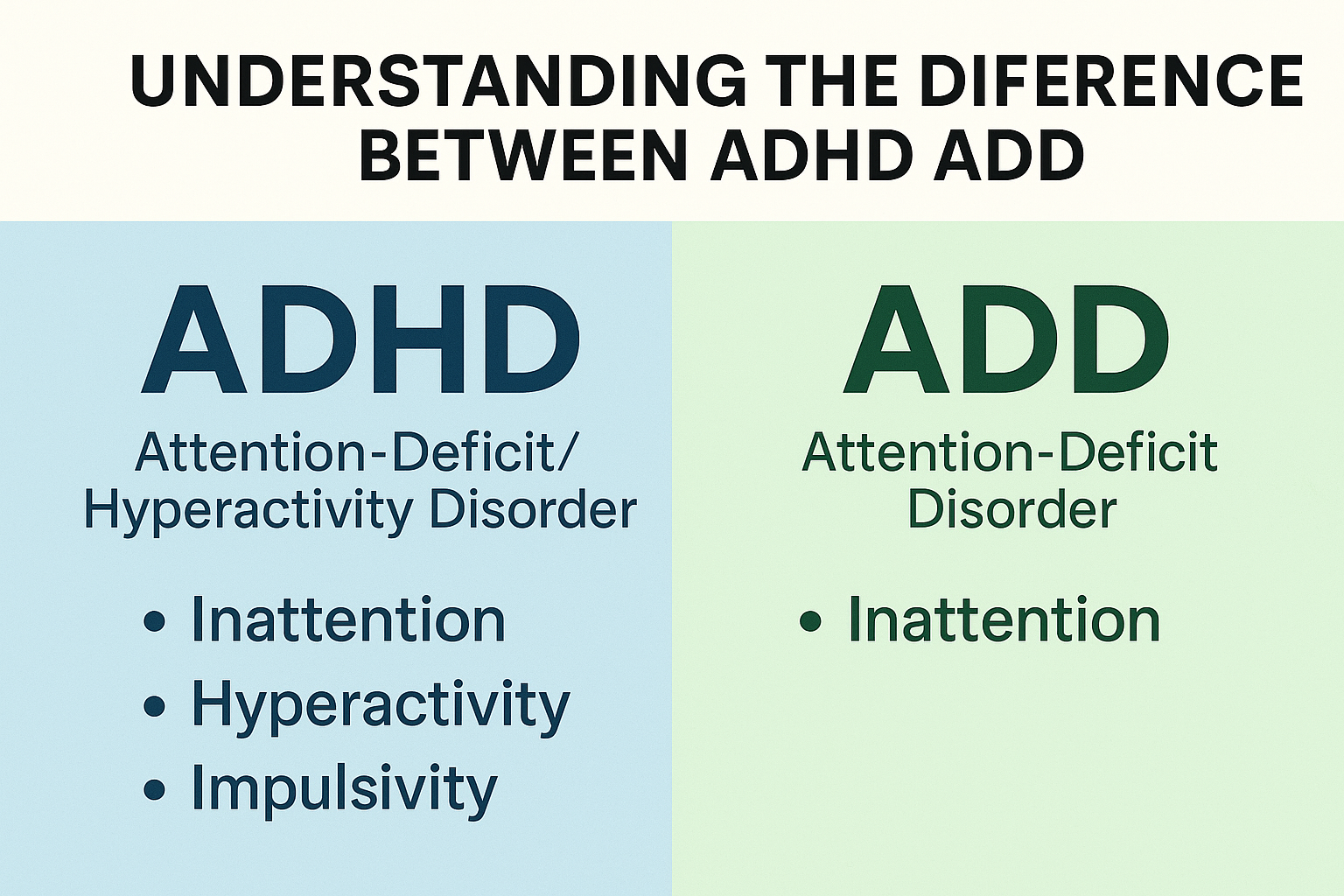
Many people search online for “ADD vs ADHD,” but often get confused by overlapping terms and outdated definitions. In fact, ADD (Attention‑Deficit Disorder) is an older, informal term, and the correct clinical term now is ADHD (Attention‑Deficit/Hyperactivity Disorder). In this article, we will clarify the difference, explain why ADD is no longer used diagnostically, explore the various presentations of ADHD, and show how occupational therapy can support individuals across these variations.
- Why the Term “ADD” Is Outdated
- Originally, the DSM‑III (1980) used the term ADD (Attention‑Deficit Disorder) to describe attention difficulties, whether or not hyperactivity was present (i.e. “with or without hyperactivity”).
- In 1987, when the DSM‑III‑R was published, medical professionals shifted the terminology to ADHD (Attention‑Deficit/Hyperactivity Disorder), combining attention deficits and hyperactivity/impulsivity under one umbrella.
- Today, ADD is not an official DSM diagnosis. Instead, what people often call “ADD” corresponds to the inattentive presentation of ADHD.
- Many sources confirm that ADD is now considered a colloquial term rather than a separate disorder.
So when people search “ADD vs ADHD,” the most accurate answer is: There is no separate ADD — the official term is ADHD, and it includes an inattentive subtype.
- ADHD: The Unified Clinical Term
Core Definition and Features
ADHD is classified as a neurodevelopmental disorder characterized by symptoms of inattention, hyperactivity, and impulsivity, which:
- Are excessive relative to developmental level
- Persist over time
- Occur in multiple settings (school, home, work)
- Interfere with social, academic, or occupational functioning
- Aren’t better explained by another disorder
The shift to ADHD as a unified term helps clinicians and the public understand that attention difficulties and hyperactivity often belong to the same spectrum.
Presentations (Types) of ADHD
Under the DSM‑5 (and later updates), ADHD is not separated into rigid “subtypes” but rather presentations, since symptom patterns may change over time. The main presentations are:
- Predominantly Inattentive Presentation
- This is what many people still informally call “ADD.”
- Core symptoms: trouble sustaining attention, forgetfulness, distractibility, disorganization, careless mistakes, losing things.
- Hyperactivity or impulsivity are minimal or absent.
- Predominantly Hyperactive‑Impulsive Presentation
- Symptoms of excessive motor activity, fidgeting, interrupting, restlessness, difficulty waiting turn, impulsive behavior.
- Inattention may be present but less dominant.
- Combined Presentation
- A mix of inattentive and hyperactive‑impulsive symptoms, both reaching clinical thresholds.
Because presentations can evolve, a person diagnosed with combined ADHD in childhood may later show mostly inattentive symptoms, for instance.
- Comparing Symptoms: Inattentive vs Hyperactive/Impulsive
Below is a side‑by‑side comparison showing how the symptom profiles differ (and overlap):
| Symptom Domain | Inattentive (ADD-like features) | Hyperactive‑Impulsive |
| Sustaining attention / focus | Difficulty maintaining focus, easily distracted, daydreaming, losing track | May start tasks but shift rapidly; less sustained focus |
| Organization & planning | Disorganization, missed deadlines, forgetting tasks | Impulsively jumping between tasks |
| Memory / forgetfulness | Frequent forgetfulness of daily tasks, misplacing items | Forgetfulness may exist but overshadowed by hyperactive behavior |
| Motor activity | Usually not excessive movement | Fidgeting, restlessness, difficulty sitting still |
| Impulsivity | Less pronounced | Blurting, interrupting, acting without thinking |
| Behavioral visibility | Often quiet or “under the radar” | More noticeable, may attract attention in class/office |
It’s important to note that many people have a combination of these traits to varying degrees.
- Why the Distinction Matters (Even Though ADD Is Outdated)
Even though ADD is no longer a formal diagnosis, understanding which symptoms predominate is critical for:
- Tailoring assessment and diagnosis — Clinicians can use symptom checklists and interviews that emphasize the relevant domain(s).
- Designing interventions — Strategies differ depending on whether the challenge is mainly inattentive or hyperactive features.
- Monitoring changes over time — Presentations can shift across childhood, adolescence, and adulthood, so interventions must adapt.
- Reducing underdiagnosis — Because inattentive ADHD is less conspicuous, many individuals (especially girls or quieter students) may not be identified or supported.
- Diagnosis: How Clinicians Distinguish Presentations
Diagnostic Criteria & Process
- A clinician uses the DSM or ICD criteria to evaluate symptoms across domains.
- A diagnosis must show a sufficient number of symptoms in the relevant domain(s), start before a certain age (traditionally before age 12), and persist across settings (home, school, work).
- Ratings from multiple observers (teachers, caregivers, self reports) and objective measures (behavior checklists, neuropsychological tests) help strengthen the diagnosis.
- Because ADD / inattentive presentation is less disruptive, it is sometimes overlooked unless assessment includes targeted questions about attention, organization, and executive function.
Comorbidities & Overlap
Many individuals have co‑occurring conditions, such as anxiety, depression, learning disabilities, or executive function deficits. These can blur the diagnostic picture and require careful differential assessment.
- Occupational Therapy & ADHD: Tailoring Support by Presentation
From the perspective of occupational therapy, knowing whether a person has more inattentive or hyperactive/impulsive symptoms helps in crafting appropriate goals and interventions.
For Inattentive (ADD‑style) Challenges
Therapy goals and strategies may include:
- Task breakdown: splitting larger tasks into smaller, manageable steps
- External scaffolding: planners, checklists, visual schedules
- Time management tools: timers, alarms, reminders
- Minimizing distractions in the environment
- Teaching self‑monitoring and prompting strategies
- Memory aids: notebooks, smartphone apps, prompts
- Developing structured routines and habits
For Hyperactive / Impulsive or Combined Presentations
Interventions might emphasize:
- Sensory modulation and movement opportunities (e.g. scheduled breaks, fidget tools)
- Self‑regulation training: pause–think–act, mindfulness, impulse control techniques
- Task design that allows movement or active engagement
- Behavior strategies: cueing, structured transitions, reinforcement
- Environmental adjustments to reduce overstimulation
- Integration of executive functioning supports
Overlap Strategies (Applicable to Both Presentations)
- Executive functioning coaching (planning, organization, working memory)
- Habit formation and consistency
- Training in metacognitive techniques (reflect, adjust)
- Collaboration with educators, caregivers, therapists for consistency across settings
- Use of assistive technology and apps
The key is customization: what works best depends on which symptom set is more disruptive for an individual.
- Practical Tips & Strategies
Here are actionable tips you can include (or share) on your website or OT practice site, optimized around terms your target audience might search (e.g. “strategies for inattentive ADHD,” “how to manage hyperactive ADHD,” “occupational therapy ADHD strategies”):
Tips for Inattentive / “ADD‑Style” Challenges
- Use visual planners and color coding
- Set alarms, timers, reminders for deadlines, transitions
- Chunk large tasks into small steps
- Reduce distractions (quiet workspaces, minimal clutter)
- Employ checklists and “end-of-task reviews”
- Teach the person to pause, review progress, and adjust
- Use external cues (sticky notes, alerts)
Tips for Hyperactive / Impulsive / Combined ADHD
- Insert movement breaks or “brain breaks” between tasks
- Use sensory supports / fidget tools thoughtfully
- Encourage active learning / hands-on work
- Teach impulse control frameworks (e.g. “stop-think-act”)
- Use structured transitions between tasks
- Reinforce good self‑control and calm behavior
Tips for Educators / Parents / Caregivers
- Provide clear, concise instructions (both written & verbal)
- Give frequent check-ins or prompts during tasks
- Use visual schedules, timers, cues in classroom or home
- Seat away from distractions (windows, screens, high-traffic areas)
- Consistently use the strategies across home, school, and therapy
- Communicate goals and methods across all stakeholders
- FAQs (Frequently Asked Questions)
Q1: Is ADD still a valid diagnosis?
A1: No. ADD is considered an outdated, colloquial term. Today, what was once called ADD falls under the umbrella of ADHD predominantly inattentive presentation.
Q2: Can someone have ADHD without being hyperactive?
A2: Yes—someone can have ADHD with primarily inattentive symptoms and little or no hyperactivity.
Q3: What are “presentations” vs “types” of ADHD?
A3: In current terminology, ADHD is described by presentations (patterns of dominant symptoms) rather than rigid subtypes. Presentations can change over time.
Q4: How does occupational therapy help people with ADHD?
A4: OT can provide personalized strategies to improve executive function, self-regulation, organization, task initiation, and daily routines—tailored to each person’s symptom profile.
Q5: Can ADHD symptoms change over time?
A5: Yes, individuals may shift from one presentation to another (e.g. combined → inattentive) as they age or as circumstances change.
- Conclusion & Key Takeaways
- The difference between ADHD and ADD is not between two separate disorders: ADD is an outdated term.
- The official clinical term is ADHD, which encompasses inattentive, hyperactive‑impulsive, and combined presentations.
- Many people still use “ADD” to refer to those who have predominantly inattentive symptoms, but clinically the label is ADHD.
- Knowing which symptoms are more prominent is crucial for assessment, diagnosis, and tailored intervention.
- Occupational therapy plays a meaningful role in supporting individuals with ADHD by targeting executive function, self‑regulation, strategies, and environment adaptation.
- Use the above strategies and tips to support clients, caregivers, educators, and learners with ADHD—in whatever presentation it appears.

2 thoughts on “Understanding ADHD vs ADD: What’s the Difference?”
Clear and helpful explanation—finally makes sense why ADD is no longer used!
Loved how you showed the OT strategies for each ADHD type. Super practical!